Gut Health Fiber Calculator
How Much Fiber Do You Need?
Your gut thrives on fiber. The article recommends 25-30g of fiber daily for optimal gut health, but most people get less than half that amount.
Add Foods to Track Your Fiber
Your Fiber Track
Top High-Fiber Foods
Try these gut-friendly foods to boost your fiber intake:
- • 1 cup of cooked lentils (15.6g fiber)
- • 1 medium apple with skin (4.4g fiber)
- • 1/2 cup of chia seeds (10.6g fiber)
- • 1 cup of cooked broccoli (5.1g fiber)
- • 1/2 cup of black beans (7.5g fiber)
- • 1/2 cup of oats (4.1g fiber)
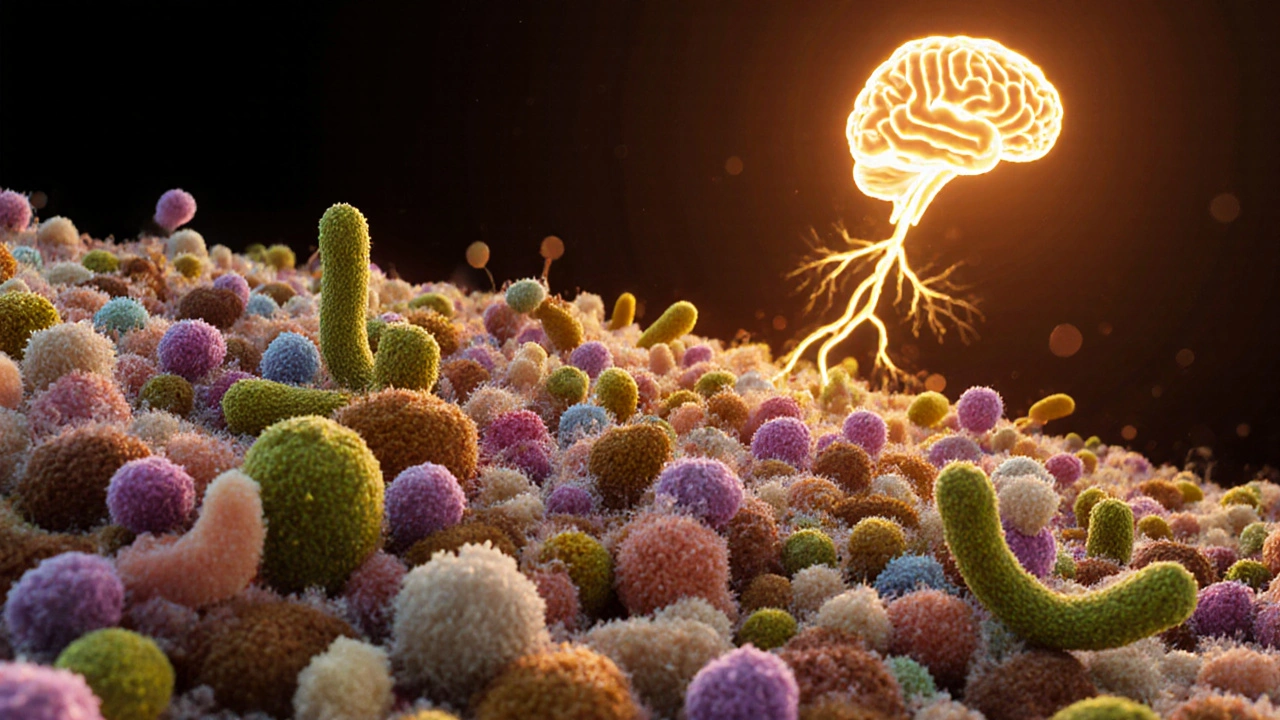
Your gut isn’t just a place where food disappears and waste appears. It’s a living, breathing ecosystem that controls everything from your mood to your energy, your immune response, and even how well your body absorbs nutrients. If your gut is out of balance, no amount of kale smoothies or protein shakes will fix what’s really wrong. This isn’t theory-it’s biology. Over 70% of your immune system lives in your gut. The trillions of bacteria living inside you communicate with your brain through the vagus nerve. When those bacteria are thriving, you feel better. When they’re struggling, you feel off-bloating, fatigue, brain fog, even anxiety.
What Exactly Is Gut Health?
Gut health means having a balanced, diverse community of microorganisms-mostly bacteria, but also fungi and viruses-living in your digestive tract. This group is called your microbiome. It’s not just about avoiding diarrhea or constipation. A healthy gut microbiome helps break down fiber, produces key vitamins like B12 and K, trains your immune system to recognize threats, and keeps harmful bacteria from taking over.
Think of it like a garden. If you only plant one kind of flower, the soil gets weak. Pests move in. The whole system collapses. Your gut works the same way. Eating the same processed foods day after day wipes out the good bacteria. They starve. The bad ones take over. And suddenly, you’re dealing with bloating after meals, sugar cravings you can’t shake, or skin breakouts that won’t go away.
The Gut-Brain Connection Is Real
You’ve probably heard of the ‘gut feeling.’ That’s not just a metaphor. Your gut and brain are wired together. The gut produces about 90% of your body’s serotonin-the chemical that helps regulate mood, sleep, and appetite. When your gut bacteria are unhealthy, serotonin production drops. That’s why people with chronic gut issues often report depression or anxiety. A 2023 study in Nature Microbiology found that people with irritable bowel syndrome (IBS) had significantly lower levels of certain bacterial strains linked to calmness and emotional balance.
It goes both ways. Stress doesn’t just make you feel anxious-it physically changes your gut. High cortisol levels slow digestion, reduce blood flow to the intestines, and kill off beneficial bacteria. That’s why you get stomachaches before a big presentation or lose your appetite during a breakup. Your gut doesn’t just react to what you eat. It reacts to what you feel.
What Kills Your Gut Health?
Not all foods are created equal when it comes to feeding your microbiome. Here’s what actually damages it:
- Refined sugar-feeds harmful yeast and bacteria, leading to inflammation and leaky gut.
- Artificial sweeteners-studies show they alter gut bacteria in ways that increase glucose intolerance, even without calories.
- Processed vegetable oils-like soybean and canola oil-promote inflammation and disrupt the gut lining.
- Antibiotics-even one course can wipe out 30% of your gut bacteria, and some strains never fully recover.
- Chronic stress-lowers stomach acid, slows digestion, and weakens the gut barrier.
These aren’t just ‘bad habits.’ They’re direct attacks on your microbial ecosystem. And the damage isn’t always obvious. You might not have diarrhea, but you could be silently absorbing fewer nutrients, storing more fat, or fighting off constant low-grade inflammation that leads to weight gain, joint pain, or brain fog.
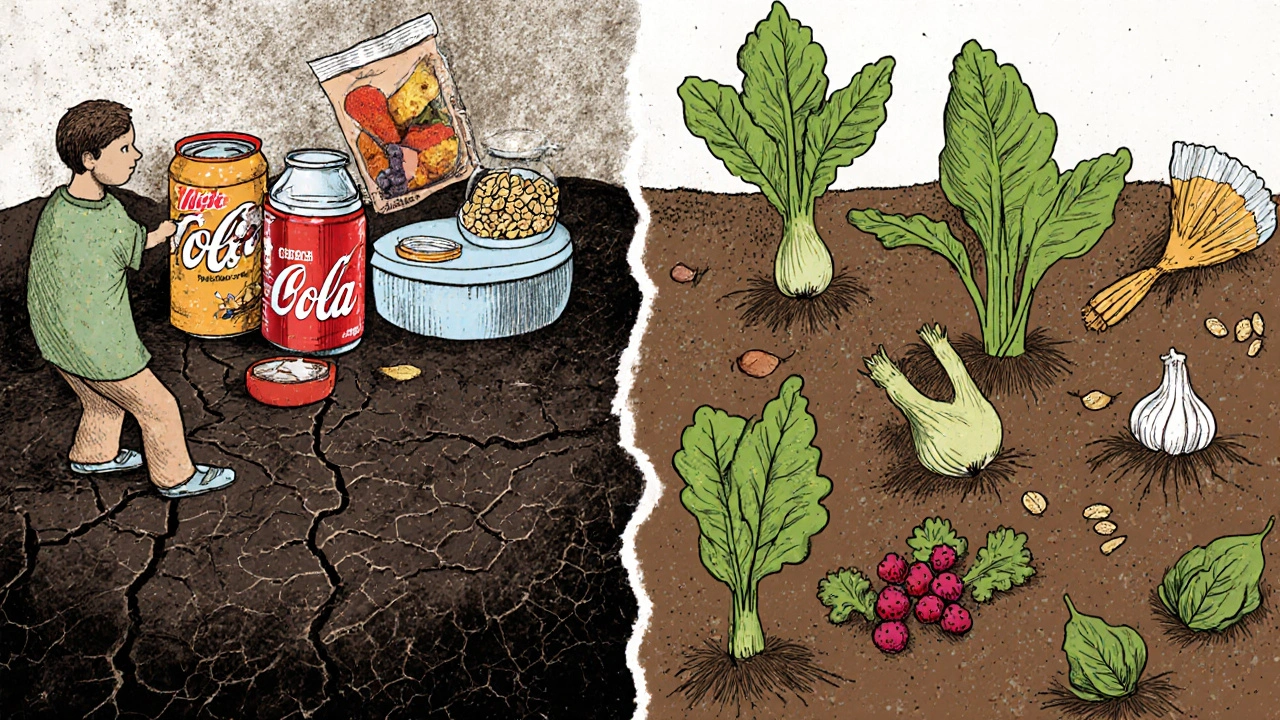
How to Fix It: Food That Heals
The good news? Your gut can heal. And it doesn’t require expensive supplements or extreme diets. It starts with what’s on your plate.
Probiotic-rich foods introduce live beneficial bacteria. Think: plain yogurt with live cultures, kefir, sauerkraut, kimchi, miso, and kombucha. Don’t buy pasteurized versions-they kill the good bacteria. Look for ‘raw’ or ‘naturally fermented’ on the label.
Prebiotic foods feed the good bacteria you already have. These are fibers your body can’t digest but your gut microbes love. Garlic, onions, leeks, asparagus, bananas, oats, flaxseeds, and dandelion greens are top choices. Aim for at least 25-30 grams of fiber daily. Most people get less than half that.
Also, eat more polyphenols-plant compounds that act like fertilizer for good bacteria. Berries, dark chocolate (70%+ cocoa), green tea, red wine (in moderation), and olives are packed with them.
Supplements: Helpful or Hype?
Probiotic supplements can help, but they’re not magic pills. Most store-bought ones contain only 1-10 strains. Your natural gut has over 1,000. A 2024 review in The American Journal of Gastroenterology found that multi-strain probiotics (10+ strains) were more effective than single-strain ones for reducing bloating and improving stool consistency.
But here’s the catch: not all probiotics are created equal. Some die before they reach your gut. Look for brands that use delayed-release capsules or spore-forming strains like Bacillus coagulans-they survive stomach acid. Also, check the CFU count. Aim for at least 10 billion colony-forming units per dose.
Prebiotic supplements like inulin or FOS can help, but if you have SIBO (small intestinal bacterial overgrowth), they can make things worse. Always start with food first. Supplements are support, not substitutes.
What About Fasting and Gut Reset Diets?
Intermittent fasting-like eating within an 8-hour window-can give your gut a break. It allows time for the migrating motor complex (MMC), a cleaning wave in your intestines, to sweep out leftover food and bacteria. This process doesn’t happen while you’re eating. A 2022 study in Cell Metabolism showed that time-restricted eating improved microbial diversity and reduced inflammation markers in just 8 weeks.
But don’t jump into 16:8 fasting if you’re already stressed, underweight, or have a history of disordered eating. Your gut needs consistency, not chaos. A simpler approach: don’t snack all day. Give your digestive system 3-4 hours between meals. That’s enough time for the MMC to do its job.

Signs Your Gut Is Healing
You won’t wake up one day feeling ‘fixed.’ Healing takes weeks to months. But here’s what to look for:
- Less bloating after meals
- More regular bowel movements (once or twice daily, well-formed)
- Fewer sugar cravings
- Better sleep
- Clearer skin
- Improved focus and less brain fog
These aren’t random improvements. They’re direct results of a balanced microbiome. Better digestion means better nutrient absorption. Less inflammation means your body doesn’t have to work overtime to fight itself. And when your gut bacteria start producing more short-chain fatty acids like butyrate, your cells get cleaner fuel-leading to more energy and better mood.
What Not to Do
Don’t chase the latest ‘gut cleanse’ detox. These are usually just laxatives or juice fasts that strip your gut of everything-good and bad. You don’t need to flush your system. You need to rebuild it.
Don’t overdo probiotics. Taking 50 billion CFUs a day won’t make you healthier. It can cause gas, bloating, or even small intestinal bacterial overgrowth if your gut is already fragile.
Don’t ignore food intolerances. If you’re sensitive to dairy, gluten, or FODMAPs, eating them daily will keep your gut inflamed-even if you take probiotics. Healing isn’t just about adding good stuff. It’s also about removing the things that harm you.
Start Small. Stay Consistent.
You don’t need to overhaul your diet overnight. Pick one thing:
- Add fermented veggies to your lunch.
- Swap your morning cereal for oats with chia seeds and berries.
- Stop drinking soda and replace it with sparkling water and lemon.
- Don’t eat dessert right after dinner. Wait two hours.
Small changes compound. In 30 days, you’ll notice your digestion feels lighter. In 90 days, your energy might be noticeably higher. In six months, you might realize you haven’t had a cold in months.
Your gut isn’t just part of your health. It’s the foundation. Everything else-your weight, your mood, your immunity, your skin, your brain-rests on it. Fix the gut, and you fix the rest.
Can gut health affect weight loss?
Yes. Certain gut bacteria are linked to how your body stores fat and regulates appetite. People with obesity often have less microbial diversity. Studies show that when people lose weight through diet, their gut microbiome shifts toward a healthier profile. But if your gut is inflamed or imbalanced, your body may hold onto fat even on a calorie-restricted diet. Healing your gut can make weight loss easier by reducing cravings, improving insulin sensitivity, and lowering inflammation.
Are probiotic supplements necessary?
Not for everyone. If you eat a varied diet rich in fiber and fermented foods, you likely don’t need them. But if you’ve taken antibiotics recently, have chronic digestive issues, or struggle to eat enough prebiotic foods, a high-quality probiotic can help jumpstart recovery. Look for multi-strain formulas with at least 10 billion CFUs and delayed-release capsules. Always pair them with prebiotic foods for best results.
How long does it take to heal your gut?
Some people feel better in 2-4 weeks with dietary changes. But full microbial recovery can take 3-6 months. It depends on how long the damage lasted, your age, stress levels, and how consistent you are. Think of it like reforesting a burned forest. You can’t plant trees and expect a forest overnight. You need time, consistency, and the right conditions.
Can stress really damage your gut?
Absolutely. Chronic stress lowers stomach acid, slows digestion, and weakens the gut lining-making it easier for toxins and bad bacteria to leak into your bloodstream. This triggers inflammation, which can lead to food sensitivities, autoimmune reactions, and brain fog. Managing stress through sleep, movement, or breathing exercises isn’t optional-it’s part of gut healing.
Is a gluten-free diet good for gut health?
Only if you have celiac disease or a diagnosed gluten sensitivity. For most people, gluten itself isn’t the problem-it’s the processed foods that contain it, like white bread, cookies, and crackers. These foods are low in fiber and high in sugar and unhealthy fats, which harm your microbiome. If you cut out processed grains and replace them with whole grains like oats, quinoa, or brown rice, your gut improves-not because you avoided gluten, but because you ate better food.
What’s the difference between prebiotics and probiotics?
Probiotics are live beneficial bacteria you consume-like in yogurt or supplements. Prebiotics are the fiber that feeds those bacteria. Think of probiotics as the seeds and prebiotics as the soil and fertilizer. You need both. Without prebiotics, probiotics can’t survive long-term. Without probiotics, prebiotics have nothing to nourish. They work together.





